
 One of the most frustrating group of patients for IVF specialists are those with recurrent implantation failure. These are patients for whom we've done multiple IVF cycles but who still do not get pregnant.
One of the most frustrating group of patients for IVF specialists are those with recurrent implantation failure. These are patients for whom we've done multiple IVF cycles but who still do not get pregnant.
These patients as labeled as having "repeated IVF failure" or "recurrent implantation failure". In reality, these are just bucket diagnoses which means we really do not know why the embryos we transfer do not implant for these women.
On an intellectual level, we understand that there are broadly only two groups of reasons for failure of implantation. One could be that the embryos are not of good quality. The other is that there is a problem with endometrial receptivity. Unfortunately, because it is still very difficult for us to pinpoint what the problem is in an individual patient, there is a lot of hocus-pocus and mystery surrounding the treatment options for these patients.
They are emotionally very vulnerable and very desperate. They will often keep on changing doctors, and each new doctor will offer his own particular flavor of some magic potion in order to solve the problem. This could range from using intravenous Intralipids; to doing PGD for comprehensive chromosomal screening; to using immunotherapy for treating NK (natural killer) cells.
A lot of this is extremely speculative stuff and I feel a better treatment option would be one which is based on sound science. This would be to grow all the embryos to blastocyst stage; freeze all of them, and then transfer them in the next cycle. While this may seem to be a lot of hard work, there is a sound scientific basis to this approach.
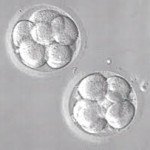
Growing embryos to blastocyst stage (rather than transferring them on Day 2 or 3) is the best way we have today of ensuring that the embryos are competent. While it's true that not all blastocysts are genetically normal (which is why not all of them will implant), given the state of the technology available today, this is the best approach we have for making sure that the embryos are viable.
If the embryos do not grow up to the blastocyst stage, this means that means the problem for recurrent implantation failure is quite likely to be an embryo problem. This is especially true when patients with recurrent implantation failure have had multiple failed IVF cycles with only Day 2 or Day 3 transfers, and the earlier IVF clinic has not tried to grow their embryos to the blastocyst stage.
While the fact that their embryos have arrested in vitro and have failed to develop to blastocysts (which means they will not have any embryos to transfer at all) can break their heart, at least this way they know where the problem lies, so they can then approach their next treatment cycle armed with more intelligence . This approach provides valuable information, rather than leave patients groping in the dark.
Why not transfer the fresh blastocysts? This is because endometrial receptivity may be suboptimal in a super ovulation cycle thanks to all the hormones which have been injected. Because the thrust of superovulation is to focus on growing good-quality eggs, sometimes we may not be able to optimize endometrial receptivity at the time at which the eggs are ready for retrieval.
Once we have frozen all the blastocysts, we can then focus all our energies in the next cycle on improving endometrial receptivity. This approach allows us to maximize the chances of implantation, because we are transferring good-quality blastocysts into an optimally prepared endometrium.
This approach allows us to use sound scientific principles without resorting to a lot of expensive hocus-pocus to maximize chances of success. Only very skilled IVF labs can offer this kind of service, because it needs a lot of expertise and experience to do this successfully.
To see a fertility specialist who is a board-certified physician with excellent success rates, make an appointment at one of InVia’s four Chicago area fertility clinics.

Dr. Aniruddha Malpani is an IVF specialist with a brilliant career with numerous awards, educational distinctions and prizes. Dr. Malpani completed his postgraduate degree in Gynecology from the University of Bombay in 1986. He received further training in IVF from UCSF, San Francisco, and U.S.A. As a medical student, he studied at Harvard, Johns Hopkins and Yale. He practices in Mumbai, India along with his wife Anjali. He can be contacted at info@drmalpani.com, or learn more at http://www.drmalpani.com.
Subscribe to our weekly blog digest

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists

Comments