is a test commonly used for testing ovarian reserve. AMH levels reflect the number of eggs (oocyte pool) that remain in the ovary(ies). AMH levels will decline as a woman ages. AMH levels also indicate the number of eggs that will be retrieved and IVF pregnancy rates – a high number is associated with a better outcome. In many IVF clinics, an AMH level > 1.0 ng/mL is considered normal. At InVia we like our anonymous egg donors to have an AMH level > 1.5 ng/mL. Low AMH levels, on the other are associated with a low number of eggs retrieved and a lower pregnancy rate. There are several physicians who will recommend using an egg donor to patients based on low AMH levels alone. If this is a correct policy, it will save a lot of money for the health system. If it is incorrect, then these patients are being treated unfairly. So, it is logical to ask, “What are the pregnancy rates in women with low AMH levels?”
 Anti-mullerian hormone (AMH) level
Anti-mullerian hormone (AMH) level
This very issue was addressed by Kedem et al. in a recent publication (Kedem A, Haas J, Geva LL, Yerushalmi G, Gilboa Y, et al. (2013) Ongoing Pregnancy Rates in Women with Low and Extremely Low AMH Levels. A Multivariate Analysis of 769 Cycles. PLoS ONE 8(12): e81629. doi:10.1371/journal.pone.0081629). Here are their findings.
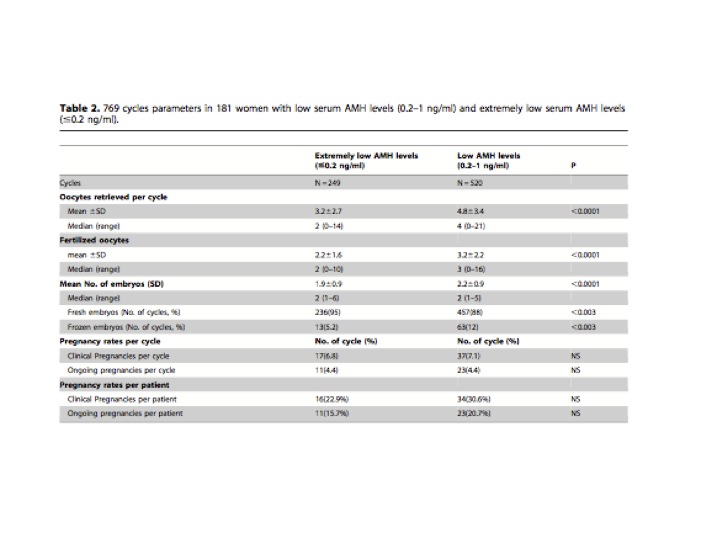
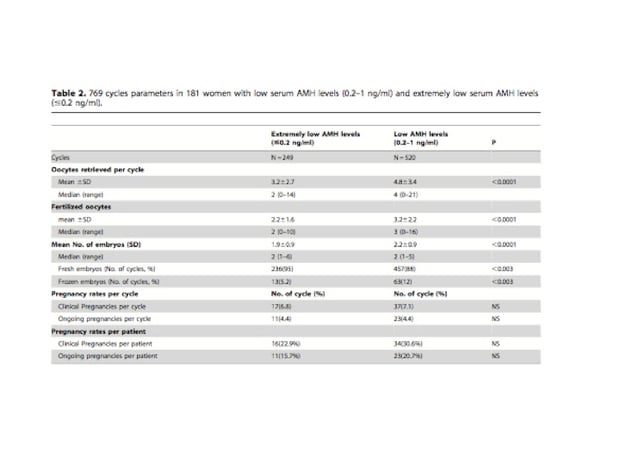
They analyzed data from 70 patients undergoing 249 cycles with extremely low AMH levels (≤ 0.2 ng/mL) and an additional 111 patients undergoing 520 cycles with low AMH levels (0.21 – 1.0 ng/mL). Number of oocytes (eggs) retrieved per cycle, fertilized oocytes and number of transferred embryos were significantly lower in the extremely low AMH levels group compared to the low AMH levels (P < 0.003). Crude ongoing pregnancy rates were 4.4% for both groups of patients. Among 48 cycles of women aged ≥ 42 with AMH levels of ≤ 0.2 ng/ml no pregnancies were observed. But, in patients with AMH levels of 0.2–1.0 ng/ml, 3 ongoing pregnancies out of 192 cycles (1.6%) were observed. However, in a multivariate regression analysis adjusted for age and cycle characteristics, no significant differences in ongoing pregnancy rates per cycle between the two groups were evident. Cumulative pregnancy rates of 20% were observed following five cycles, for both groups of patients. There were 34 ongoing pregnancies in 769 cycles, 181 women.
It is not clear from the manuscript if these patients were all stimulated with an aggressive stimulation protocol (FSH/hMG daily dose of 450 – 600 units). They also have not specified the cycle cancellation rate. The numbers of eggs retrieved were indeed really low (see table). The group with extremely low levels of AMH had an average retrieval of 3.2 oocytes per cycle with 65% of the cycles producing 3 or less oocytes per cycle, as compared to 4.8 oocytes retrieved per cycle in the group with low AMH levels where 42% of the cycles produced 3 or less oocytes per cycle. However, only 8% of the cycles in those with extremely low AMH levels had 5 or more fertilized oocytes per cycle versus 25% in cycles of patients with a low AMH. The fertilization rate was similar between the groups (68% and 66% respectively). Overall, 115 cycles (22%) produced no embryo for transfer in the low AMH group as compared with 81 cycles (32%) where no embryo was available for transfer in the extremely low AMH group (P < 0.001). The average number of embryos for transfer was 1.960.9 and 2.260.9, respectively for the 2 groups (P < 0.0001). Nevertheless, there were no significant differences in the clinical and ongoing pregnancy rates per cycle between the extremely low and the low AMH groups (6.8% and 4.4% vs. 7.1% and 4.4%, respectively) or in the clinical and ongoing pregnancy rates per patient (23% and 16% vs. 30% and 20%, respectively).
Of interest is the fact that in Israel, IVF cycles are fully covered by the National Health Service insurance, and there are no financial constraints for patients to discontinue treatment.
The assay used in this study to measure AMH was the old Diagnostic System Lab (DSL) assay. This assay is no longer used. The current assay available is the Generation II assay and it measures AMH level 39% higher than the old assay i.e. an AMH level of 1.0 with the DSL assay will read 1.39 with the AMH Generation II assay. More on this in a follow up blog.
So, to conclude; with extremely low AMH levels, the ongoing pregnancy rate per cycle is around 4.4% and after 5 attempts, the cumulative pregnancy rate will be about 20%.
Infertility treatment IVF InVia Fertility Specialists Diminished ovarian reserve

Dr. Karande is Board Certified in the specialty of Obstetrics and Gynecology as well as the subspecialty of Reproductive Endocrinology and Infertility. He is a Fellow of the American College of Obstetricians and Gynecologists and Member of the American Society for Reproductive Medicine.
Subscribe to our weekly blog digest

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists

Comments