For successful implantation to occur, an embryo needs a “receptive” uterine lining (endometrium). A thin endometrium can result in lower implantation of the embryo. In previous blogs, Katie Koss and Janet Chiarmonte have discussed the various pathologies that can prevent implantation and the three common techniques used to evaluate the uterine cavity. In this blog, the thickness of the endometrial lining and measurement of the lining during cycle monitoring will be discussed.
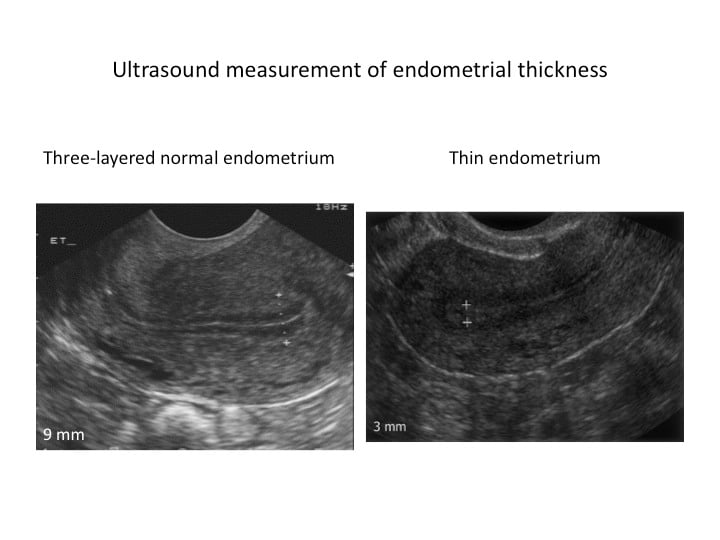
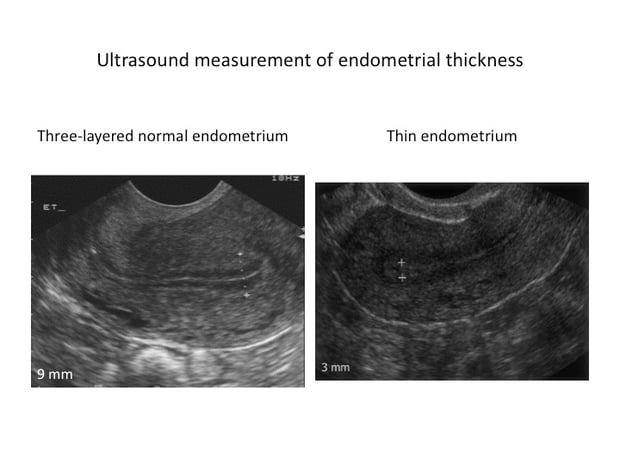
The endometrium responds to estrogen by growth in its glands and the surrounding tissue (stroma). This is reflected on ultrasound by an increase in thickness and formation of a triple-line endometrial pattern. When ovulation occurs, or when progesterone is started, a “secretory” change occurs in the endometrium, which then becomes receptive for implantation.
There is no definite cut-off level below which implantation will not occur. The consensus seems to be >7 mm in cross-section, with a triple-line endometrial pattern. An endometrial thickness <6 mm is associated with a lower rate of full-term pregnancy. Other publications suggest that thickness >9 mm is important.
Several theories have been proposed to answer this very important question
In a recent publication (Fertil Steril 2011;96:519-521), Dr. Robert Casper from the University of Toronto, Canada offers an interesting mechanism by which a thin lining results in lower implantation. The uterine lining has two layers, a “functional” layer which gets shed with menstruation and a “basal” layer which persists. The functional layer of the endometrium has plenty of small blood vessels (capillaries), in contrast to the larger spiral arteries in the basal layer.
With ovulation, there is constriction of the spiral arteries with reduced blood flow to the functional layer. This results in reduced oxygen tension, which is good for embryo implantation. In the endometrium, when the thickness measured by ultrasound is <7 mm, it is the functional layer that is thin or absent, and the implanting embryo would be much closer to the spiral arteries and the higher vascularity and oxygen concentrations of the basal endometrium. The high oxygen concentrations near the basal layer could be detrimental compared with the usual low oxygen tension of the surface endometrium.
To see a board-certified fertility specialist who uses state of the art technology to help patients get pregnant, make an appointment at one of InVia’s four Chicago area fertility clinics.
Infertility Infertility treatment IVF InVia Fertility Specialists

Dr. Karande is Board Certified in the specialty of Obstetrics and Gynecology as well as the subspecialty of Reproductive Endocrinology and Infertility. He is a Fellow of the American College of Obstetricians and Gynecologists and Member of the American Society for Reproductive Medicine.
Subscribe to our weekly blog digest

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists

Comments