We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
Adenomyosis is a gynecological disease where the glands from the lining of the uterine cavity (endometrium) are present within the uterine musculature (myometrium). Historically, adenomyosis was considered to be typically present in women who have had children (multiparous), with heavy menstrual bleeding and aged more than 40 years.
Recent advances in imaging techniques have led to adenomyosis being diagnosed in younger women who present with abnormal uterine bleeding (AUB), infertility or pelvic pain. It has even been found in women with no symptoms at all.
The typical symptoms include abnormal uterine bleeding (AUB), painful periods (dysmenorrhea), pain with intercourse (dyspareunia), chronic pelvic pain, infertility, recurrent pregnancy loss, local pressure symptoms and (rarely) bladder symptoms or indigestion (see Table 1).
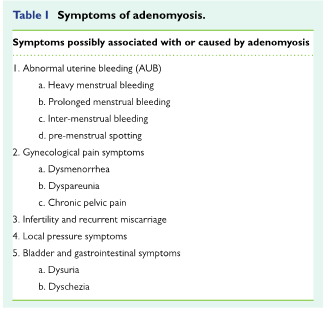
There are no symptoms that are exclusive to a diagnosis of adenomyosis. Sometimes there are other conditions that can exist along with adenomyosis (fibroids, endometriosis, endometrial polyps (usually non-cancerous growths in uterine cavity), thickening of lining of uterine cavity (endometrial hyperplasia) and make the diagnosis difficult. Like endometriosis, adenomyosis can look like many different things.
Let us discuss what some of the most common symptoms are.
Heavy menstrual bleeding is seen in about 50% of women with adenomyosis. This can last several days and can arrive at irregular times (see Table 1 above for more about what constitutes "abnormal" bleeding).
Pain can be with periods (dysmenorrhea) or there can be chronic pelvic pain. The severity of the disease is often correlated with the amount of pain experienced by the woman.
Adenomyosis can cause many difficulties with getting and staying pregnant. Infertility and miscarriages are related to the severity of the disease (localized—concentrated in one area, or diffuse—present throughout the uterus) and presence of other diseases such as endometriosis.
IVF pregnancy rates are lower in patients with adenomyosis. Some studies have also shown an increased risk of miscarriage with IVF in patients with adenomyosis. Pregnancy complications will also increase in patients with diffuse adenomyosis. These include:
There are several mechanisms that may be responsible for these complications. These include local inflammation, increased local production of prostaglandins, altered uterine contractility and defective blood vessel development.
What we find in an examination will vary based on the severity and location of the disease. A pelvic exam can often show an enlarged uterus with localized tender areas. Clinical examination may also raise suspicion of other conditions like fibroids and endometriosis. These findings are non-specific. Usually, we need to use imaging techniques to make a diagnosis of adenomyosis.
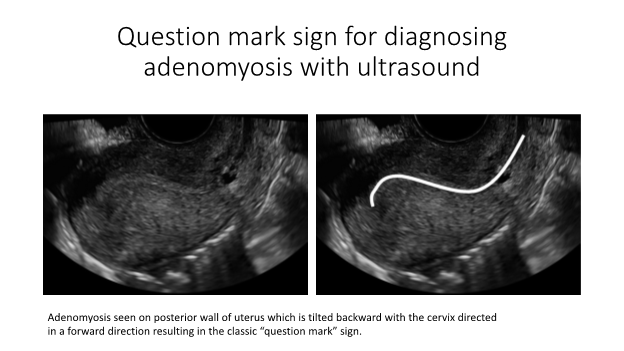
Two-dimensional and three-dimensional ultrasound can be used to diagnose the presence of adenomyosis. The findings vary based on the extent (focal or diffuse) of the disease and presence of other associated conditions (fibroids, endometriosis). 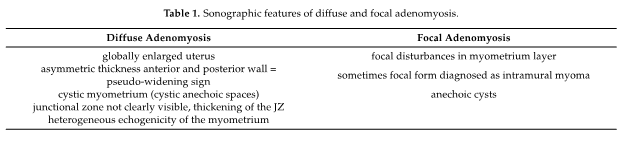
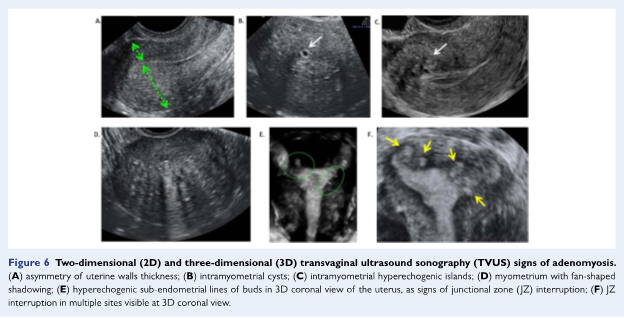
A typical ultrasound finding in patients with adenomyosis is the presence of the “question-mark” sign.
In patients with AUB, hysteroscopy can be useful as it enables one to assess the uterine cavity for abnormalities. Adenomyosis can be suspected when there are increased blood vessels seen on the uterine lining. Other findings include an irregular lining with small openings (known as the “strawberry pattern”) and submucous cysts. A biopsy of the lining can be helpful to diagnose adenomyosis. This involves using a special instrument (loop electrode with diathermy or a utero-spirotome device) to get a deep biopsy that includes the uterine musculature.
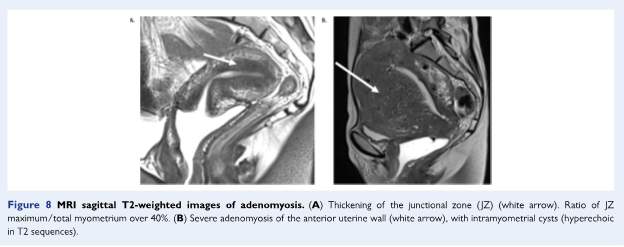
An MRI is the reference standard for diagnosing adenomyosis. It is expensive but is non-invasive. It better predicts adenomyosis when done in the secretory (after ovulation) phase of the menstrual cycle. In an MRI, we will look at an area known as the junctional zone—where the lining of the uterus (endometrium) meets the muscles of the uterine wall (myometrium).
The agreement is that a junctional zone of more than 12 mm in width is strongly associated with the disease. When the JZ measures 8–12 mm, we look to determine whether there is more than 5 mm difference between the maximum and minimum thickness of the JZ, poor definition of borders of the JZ or high-signal intensity foci in the myometrium.
There are several ways in which adenomyosis can cause infertility. These include:
As you can see, adenomyosis can have significant negative impact on fertility, potentially affecting chances of conception, implantation, and progression to a safe live birth.
Adenomyosis is a difficult clinical situation, but treatment is possible. Our team of board-certified fertility doctors can help. We have four convenient Chicago-area locations and extensive experience helping patents with fertility caused by this condition. Click below to make your appointment with InVia Fertility Specialists today.

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
