We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
The world has now been living with COVID for over a year. Over one hundred million infections have been documented, and over two and a half million people are known to have died from COVID.
During this time, it has become clear that certain populations are more at risk for severe disease and death following infection with COVID. Among these groups are pregnant women.
While most pregnant women who contract COVID will do well, pregnant women are at increased risk of severe disease, hospitalization, need for mechanical ventilation and death (references 1-5).
COVID infection may also increase risks of miscarriage in the first trimester, and prolonged high fever during the first trimester of pregnancy may be associated with the development of birth anomalies.
For the pregnancies of women contracting COVID, there is an increased risk of preterm delivery and cesarean section, and fetal deaths have occurred as well (reference 6).
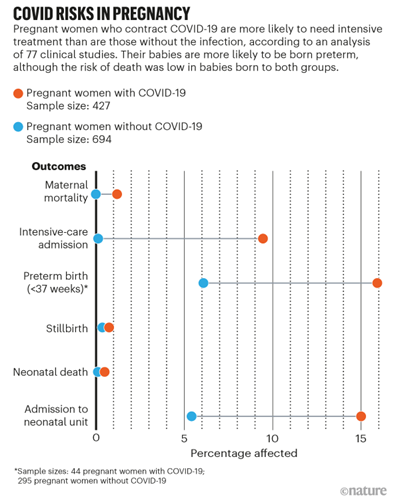
The figure above graphically represents these risks (reference 7). Women who have other risk factors in addition to pregnancy are at even greater risk of negative outcomes. These risk factors include underlying conditions such as obesity, hypertension, diabetes and asthma. Taken together, women who are pregnant or attempting pregnancy should do all they can to prevent infection with COVID, and vaccination has emerged as an important tool to achieve this goal.
Until recently, the only ways to avoid COVID infection were by means of mitigation strategies. These have included social distancing, mask wearing, limiting sizes of gatherings and hand washing. Fortunately, the last few months have seen the rapid approval of a number of safe and effective vaccines against COVID.
While mitigation strategies will continue to be important in controlling the spread of the virus, vaccinations will take on an increasingly more critical role in bringing an end to the pandemic.
Of utmost priority for women who are considering becoming pregnant is safety – for their pregnancy and for themselves. The question becomes how to best achieve this safety and how to best incorporate vaccinations into this calculation.
In thinking about whether or not to be vaccinated, it is important to consider the very real risks to a woman and her pregnancy from contracting COVID during pregnancy with the largely theoretical risks of vaccination.
The best time to take the COVID vaccine is prior to pregnancy. This allows women to become pregnant with much less worry about the risks of infection to themselves and their pregnancies. If not possible, vaccination is definitely still an option at any time during pregnancy.
In the United States, the American College of Obstetrics and Gynecology (ACOG), the American Society for Reproductive Medicine (ASRM) and the Society for Maternal Fetal Medicine (SMFM) have all advocated for vaccination of women who are pregnant, contemplating pregnancy or lactating (references 8,9,10).
The Association of Reproductive and Clinical Scientists (ARCS) and the British Fertility Society (BFS) have stated that there is no known risk from administering non-live vaccines to women who are pregnant or contemplating pregnancy (reference 11).
No. Vaccination does not cause infertility. The currently approved vaccines work via several different mechanisms, but all of them have one reassuring factor in common. The vaccines themselves induce an immune response but then disintegrate very quickly, usually in a matter of days.
The vaccines do not travel far beyond the site of injection, usually the upper arm. The antibodies that are formed do not bind to the uterus or the ovaries and are not known to affect fertility.
The answer to this is a resounding NO. There is no COVID virus in any of the vaccines currently available in Europe or the United States and there is no possibility of contracting COVID from the vaccination.
No. There is no need to wait to get pregnant after taking the vaccine. Additionally, women who have become pregnant after receiving the first vaccine of a two vaccine series should get the second vaccine during pregnancy.
There are no known risks to pregnancy from the vaccine. Some women will have a fever for a day or two. There is a theoretical risk of birth defects from very high fevers, and it is recommended that pregnant women who experience fever after vaccination take medication to lower their fever.
It is important to note that there is a much increased risk of fever from actual COVID infection, and that such fevers can be quite high and last for many days. In the balance, it is much safer to become vaccinated than risk becoming infected with all of the associated risks during pregnancy.
Beyond the benefits of maintaining maternal health during pregnancy and decreasing the risk of premature delivery which can negatively affect children, there are additional potential benefits to vaccination during pregnancy. Studies are starting to emerge that suggest that antibodies cross the placenta and can be transferred to the fetus, giving some protection against this virus to the newborn.
Similarly, antibodies can likely pass from mother to child during lactation, thereby providing another potential way for newborns to receive some protection from infection (references 12-14). These transfers of antibodies from mother to child are known as “passive immunity” whereby the baby receives the benefit of vaccination without receiving the vaccine itself.
Fortunately, most newborns do not have severe disease after infection with COVID, but there have been newborns requiring extended stays in neonatal intensive care units. Any protection that can be given to newborns, who will not be eligible for vaccination in the near future, is of potential benefit.
As has been the case with all prior vaccines, the initial COVID vaccine trials excluded pregnant women and those who were intending to become pregnant. There were a small number of patients who did become pregnant during the vaccine trials, and there were no increased risks for these women and no difference in pregnancy outcomes.
Since the vaccines have become available to a broader public, over 20,000 women in the United States alone have received a COVID vaccine during pregnancy, and there have been no increased risks noted either for the women or their pregnancies.
Fortunately, studies in pregnant women are now being undertaken. Additional information will be available to women contemplating vaccination prior to or during pregnancy in the coming months that should provide the reassurance they seek to further increase confidence in the safety of these vaccines.
The COVID pandemic has plagued the world for over a year, and it will continue to be with us for the near future. While mitigation strategies such as social distancing and mask wearing will continue to be crucial in preventing infection, vaccination has emerged as the primary method to protect individuals against severe disease, hospitalization and death.
Given that pregnant women face increased risk for these negative outcomes, vaccination should be prioritized for all women who are contemplating pregnancy or already pregnant. Vaccination is the best way for women to take control of their health during pregnancy and ensure the best possible outcomes for themselves and their babies.
If you want further information about COVID vaccination, fertility and pregnancy, I've included a list of scientific references I used to write this article below. If you're in the Chicago area, you can also make an appointment to consult with me or my colleagues at InVia Fertility. We are here to help on your pathway to pregnancy—pandemic or no pandemic. Stay safe!

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
