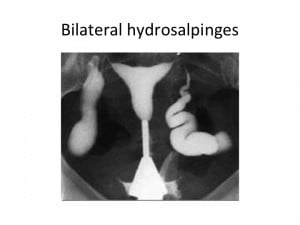
Up to 35% of female infertility is caused by tubal disease. Tubal disease is also the most obvious indication for in vitro fertilization and embryo transfer (IVF). A hydrosalpinx (hydro – “water” and salpinx – “trumpet”) is a distally blocked fallopian tube filled with serous or clear fluid. As the blocked tube distends, it develops a characteristic sausage-like shape.
Hydrosalpinges are found in 10% to 30% of patients undergoing IVF.
A hydrosalpinx can be diagnosed via transvaginal ultrasound, hysterosalpingogram, or by laparoscopy.
Patients with hydrosalpinges undergoing IVF experience approximately one-half the pregnancy rate of patients who do not have hydrosalpinges. The chances of miscarriage are also higher in this group of patients.
The poorest outcomes are in patients with hydrosalpinges large enough to be visualized on ultrasound. This reduction in success rates was noted in fresh as well as cryo-preserved embryo transfer cycles.
There are several possible explanations for the harmful effects of hydrosalpinges on IVF outcomes. 1) the hydrosalpinx fluid trickles into the uterine cavity and mechanically washes out the embryos. 2) the hydrosalpinx fluid is toxic to the embryos 3) the fluid reduces the receptivity of the uterine lining (disturbed expression of cytokines and integrins).
Removal of the tubes (salpingectomy) via laparoscopy has been shown to restore IVF outcomes in these patients.
Other options that are effective include interruption of the tubes without removing them. If the tubes are surgically correctable, then one may open up the distal end of the tube (salpingostomy).
Another way of preventing the hydrosalpinx fluid from entering the uterine cavity is by blocking them by placing an Essure device into the tubal openings via hysteroscopy.
Aspirating the hydrosalpinx fluid with a needle under transvaginal ultrasound guidance does not work. This is so because the fluid reaccumulates within two days.
So, what does this mean for you as a patient? Since, a hydrosalpinx is associated with poor fertility prognosis removing the tube is usually the best option. This decision can be based on these five factors: the extent of the adhesions, the nature of the adhesions, the diameter of the hydrosalpinx, the condition of the hydrosalpinx, and the tubal wall thickness. Whether or not you should have your fallopian tube(s) removed before IVF is something you should discuss with your physician.

Kimberly E. Saaby, has a BA in Health Care Administration, is a certified ultrasonographer, and a medical assistant. Joining the Invia team in 2001 when she began as a receptionist at the front desk where she realized the importance of spending time with patients and their needs. Her background medical experience as a patient care tech/phlebotomist at Central DuPage Hospital sparked an interest in the nursing end of the spectrum. From there she received her certification in ultrasound from Technical School and Medicine and finished her BA in Health Care Administration from University of Phoenix. She is responsible for coordinating IUI and IVF cycles, while providing patients with the education and support they need. Her knowledge extends to insurance and many other nursing activities in the clinic. When away from the clinic Kimberly enjoys the company of family and spending time outdoors with her husband, Mike.
Subscribe to our weekly blog digest

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists

Comments