So, you've been through an IVF cycle. Your doctors have retrieved a good number of eggs with a good number reaching the blastocyst stage. Having counseled about the advantages of SMART IVF, you agreed to have the embryos biopsied and the cells analyzed for chromosomal abnormalities (preimplantation genetic screening (PGS) or preimplantation genetic diagnosis (PGD)). The results showed a good number of “normal” (euploid) embryos. You then underwent embryo transfer of a single cryopreserved (frozen) euploid embryo. Everything seemed to be going well, but then, the pregnancy test result was negative! It is reasonable to ask, "Why did I have a failed IVF cycle when we transferred 'normal' embryos?"
Between 30% and 70% of human embryos are chromosomally abnormal. The number can be 100% in older patients. With SMART IVF, we are able to screen out these “abnormal” (aneuploid) embryos (sometimes, the best-looking embryos will be abnormal and vice versa). At InVia Fertility Specialists, we currently have a 70% pregnancy rate with the transfer of a single euploid embryo. But that also means that 30% of the time, patients will have to try again. To understand why even SMART IVF fails, it helps to look at data from a paper by Dr. David Meldrum at the University of California at San Diego, in Fertility and Sterility (in press):
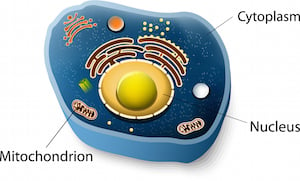
A cell consists of a nucleus, which contains chromosomes. The nucleus in turn is surrounded by a thick fluid, which fills the cell and is called cytoplasm. The cytoplasm consists of several organelles that are essential for the cell to survive. One such organelle is the mitochondria which supplies energy to the cell. Cytoplasmic quality may be sufficient to support normal chromosomal division but not to result in a fully capable embryo. As the embryo divides, each blastomere receives a smaller and smaller share of everything the egg has managed to accumulate. The embryo is not capable of adding cytoplasmic factors till it starts dividing (cleavage stage) and more mitochondria do not form till the blastocyst stage.
Mitochondrial energy is critically important for chromosomes to segregate and for cells to divide. Mitochondrial energy declines with age.
“Stressed” embryos appear to compensate by producing more mitochondrial DNA. A recent study by Simon, et al., of the University of Valencia, Spain, showed that increased mitochondrial DNA levels were associated with poor embryo capacity to implant.
Emotional stress can have a negative impact on egg quality. The “fight or flight” response associated with stress mobilizes blood flow to the heart, muscles and brain at the expense of “inessential” organs such as the ovary. The quality of blood flow to the follicles strongly correlates to pregnancy outcome. The introduction of a “mind-body” program improved IVF outcomes at a large IVF clinic in Boston run by Dr. Alice Domar.
These can take 3 – 6 months before they have an optimal effect.
Using too much or too little of stimulation medications can impact egg quality. The use of “mild” stimulation protocols in poor responders is currently being investigated at InVia.
It is very important that conditions be optimal in the embryology laboratory.
To work with a fertility clinic that uses a state-of-the art laboratory to achieve exceptional success rates, make an appointment at one of InVia's four Chicago area fertility clinics.

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
