We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
 Do autoimmune issues contribute to recurring pregnancy loss? In the February 2012 issue of the journal "Sexuality, Reproduction and Menopause", Doctors Kutteh and Odam from The University of Tennessee Health Science Center Memphis, Tennessee discuss the role of autoimmune testing in patients with recurrent pregnancy loss (RPL). Here is a brief summary of their findings.
Do autoimmune issues contribute to recurring pregnancy loss? In the February 2012 issue of the journal "Sexuality, Reproduction and Menopause", Doctors Kutteh and Odam from The University of Tennessee Health Science Center Memphis, Tennessee discuss the role of autoimmune testing in patients with recurrent pregnancy loss (RPL). Here is a brief summary of their findings.
For a pregnancy to succeed, two immunologically and genetically distinct tissues must coexist. Autoimmunity refers to an immune reaction of the body against substances that are normally present in the body. Numerous studies have attempted to identify specific autoantibodies associated with pregnancy loss. Several autoimmune factors have been investigated as possible influences on reproductive success and failure. Autoantibodies may persist for many years in the circulation as a marker of a prior autoimmune attack, but their presence does not necessarily indicate a current disease process.
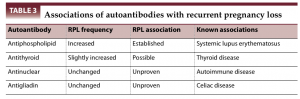
Researchers have investigated the role of autoimmune factors in women with recurrent pregnancy loss (RPL). The most commonly studied antibodies include antiphospholipid, antithyroid, antigliadin, antinuclear, antiovarian, anti-islet cell, and antisperm antibodies.
Present in an estimated 2% to 5% of the general population, antiphospholipid (aPL) antibodies are commonly associated with such autoimmune diseases as systemic lupus erythematosus, but they can also present in isolation in the form of primary antiphospholipid syndrome.
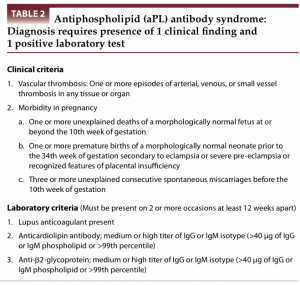
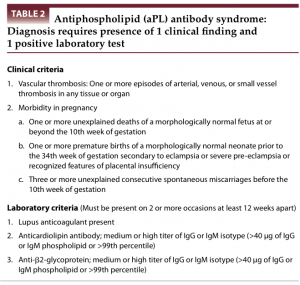
Antiphospholipid syndrome was first described in 1983 in patients with systemic lupus erythematosus, the presence of anticardiolipin antibodies, and thrombosis. The criteria for diagnosis have since been revised. For a patient to be diagnosed with antiphospholipid syndrome, at least one of the clinical criteria and one of the laboratory criteria must be met (see Table).
There are several ways in which aPL antibodies can cause miscarriages. For years, it was believed that they led to an increase in microscopic blood clots being formed in the blood vessels surrounding the pregnancy. This resulted in the pregnancy miscarrying. More recent studies suggest that aPL antibodies interfere with the process of implantation resulting in miscarriage (defective endovascular trophoblast invasion, decreased release of hCG from human placental explants, prevention of in vitro trophoblast migration and invasion, inhibition of trophoblast cell adhesion molecules, and activation of complement on the trophoblast surface inducing an inflammatory response).
Antiphospholipid antibodies have been found in 15% of patients with RPL. The treatment is a combination of heparin and low-dose aspirin. Tests for aPL antibodies include the lupus anticoagulant, and anticardiolipin antibodies.
The existence of two immunologically distinct organisms during pregnancy suggests that the immune system plays an essential role in maintaining a pregnancy. There are several other antibody tests and the current recommendations for autoimmune screening are summarized in the table below.
Alloimmune factors have been implicated as critical when associated with RPL. Sharing of HLA between partners was thought to be associated with RPL. This concept was based on a decreased maternal immune response to paternal HLA antigens and, thus, decreased production of blocking antibodies. Recent large studies, however, have found no association between HLA (and HLA-DQα) homozygosity and RPL.
Immunophenotypes of endometrial cells from women with RPL have identified certain natural killer cell (CD56+) populations. It has therefore been suggested that increased peripheral blood natural killer cells are associated with RPL. Despite the lack of diagnostic tests to identify an alloimmune factor associated with a history of RPL, abundant evidence indicates that immunologic interactions occur between the mother and her allogeneic pregnancy.
None of these factors have been clearly associated with pregnancy loss; thus, there are no recommended tests or treatments at this time. There have been several articles emphasizing that there is no good evidence for the use of intravenous gamma globulin (IVIG) therapy in a clinical setting. Use of IVIG for RPL is to be limited to approved research studies.

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
