We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
Endometriosis is a condition in which the lining of the uterus (endometrium) “escapes” and implants on structures outside the uterus. The endometrial tissue outside the uterus is affected by hormones and the menstrual cycle just like the endometrium inside the uterus. This can cause pain, heavy bleeding and other symptoms. Studies show that as many as 11% of all women in the U.S. between the ages of 15 and 44 may have endometriosis.
However, among women who have problems getting pregnant, it is possible to find endometriosis in 20% to 50% of cases. Also, the risk of infertility doubles in women over the age of 35 with endometriosis compared to women in the same age group without endometriosis. Endometriosis is thus a common cause of infertility.
But how, exactly, can endometriosis affect your fertility? There are several different effects this condition can have a person’s ability to get and stay pregnant. I will outline a few of them in this blog post.
In patients with severe endometriosis, scar tissue in the pelvis (adhesions) can involve the fallopian tubes and the resultant blockage can result in infertility. If the ovaries are trapped by scar tissue, it becomes difficult for the fallopian tubes to pick up the egg when ovulation occurs. The scar tissue can also increase the incidence of an ectopic (tubal) pregnancy.
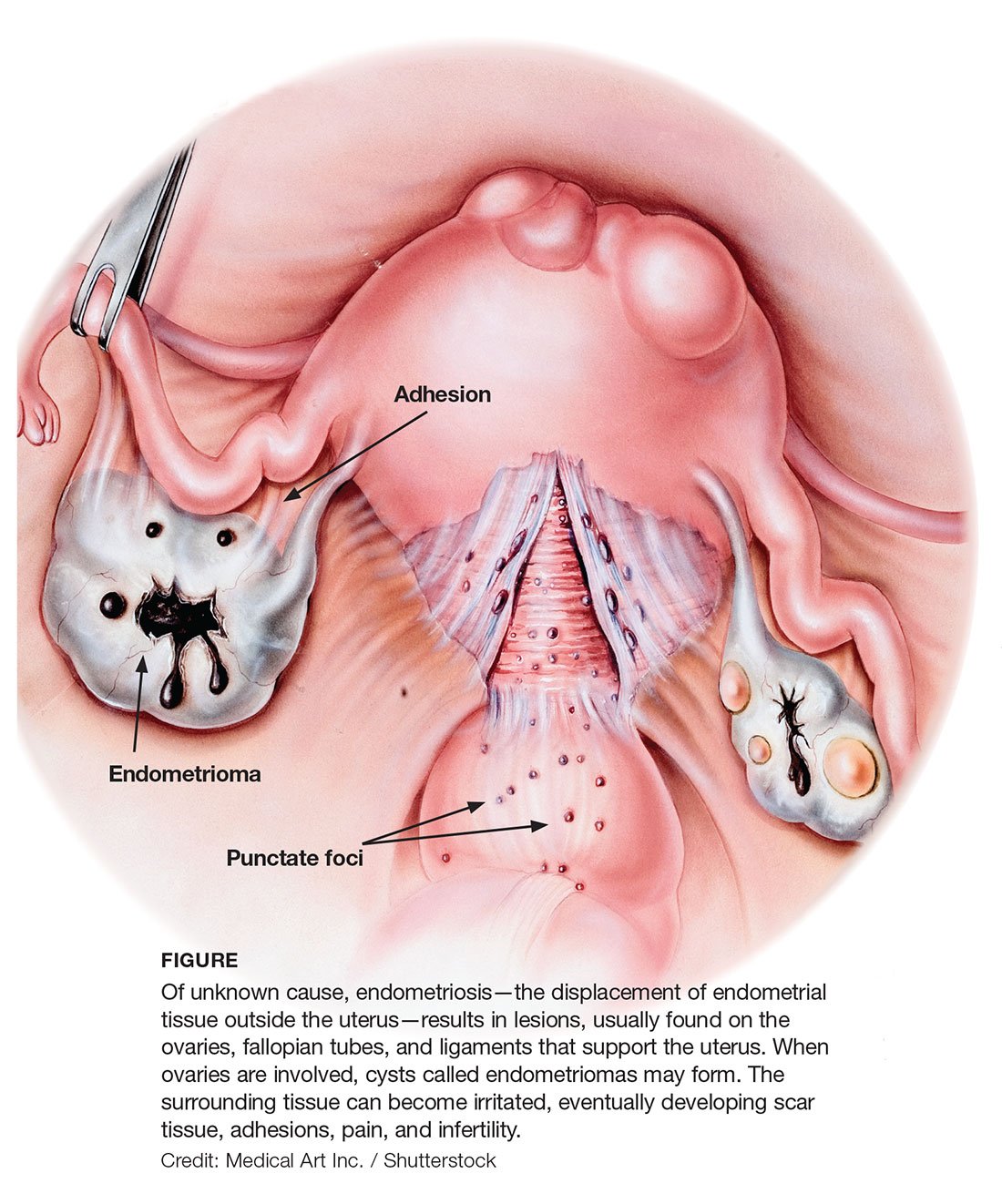
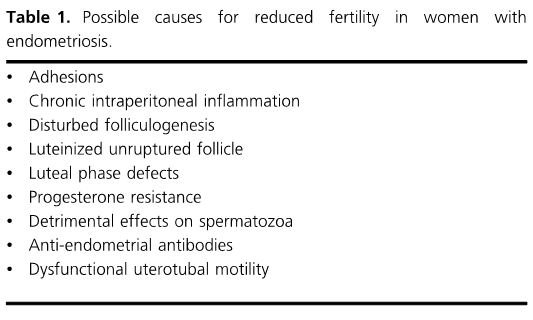
In patients with minimal or mild endometriosis, there can be several possible causes for reduced fertility (shown below in Table 1). Let us discuss some of these in detail.
Minimal or mild endometriosis is characterized by implants on the pelvic structures (see below).
 Image from a laparoscopy showing endometriosis implants (dark red) and adhesions (whitish, weblike structures)
Image from a laparoscopy showing endometriosis implants (dark red) and adhesions (whitish, weblike structures)
These implants induce an acute inflammatory reaction that activates certain immune substances (T-cells, monocytes/ macrophages) and other mediators of inflammation (cytokines, chemokines, and prostaglandins).
Essentially, the implants can trigger the body to begin the same hostile response it uses to fight off an infection or other disease, creating inflammation in the pelvic organs.
The immune response caused by the presence of endometriosis implants can impair fertility by several pathways. These include:
Endometriosis can impact the release of hormones in the brain’s hypothalamus. When the hypothalamus fails to function properly, the pituitary gland and ovaries will also not respond well. This chain reaction can negatively impact the quality of ovulation.
This interaction between the hypothalamus, pituitary gland and ovaries (called the “hypothalamic-pituitary-ovarian axis”) can also negatively impact egg quality. This disruption can also negatively impact implantation by affecting how receptive the uterine lining is to an embryo.
.jpg?width=502&name=FSi7yib%20(1).jpg) The hypothalamic-pituitary-ovarian axis, which can be affected by immune products and inflammation caused by endometriosis
The hypothalamic-pituitary-ovarian axis, which can be affected by immune products and inflammation caused by endometriosis
This is a condition where the ovarian follicle fails to rupture and release the egg. It is diagnosed by repeated ultrasound scans and occurs more often in patients with endometriosis. LUF can also be caused by pain pills (anti-inflammatory drugs like Motrin and Advil) that are often prescribed for managing menstrual pain.
Endometriosis patients can have reduced progesterone secretion after ovulation. This can lead to infertility. Many leading experts now do not believe “luteal phase defects” to be a cause of infertility.
Endometriosis is associated with reduced expression of progesterone receptors which in turn may cause progesterone resistance. (You may remember that I recently discussed a new non-surgical, non-invasive test, the ReceptivaRX™ assay, for diagnosing endometriosis. The ReceptivaRX test picks up on this issue of progesterone resistance.)
Uterine and tubal muscles play an important role in transporting sperm, eggs and embryos. Endometriosis, either in the form of adhesions or implants, can interfere with the way these muscles contract, leading to infertility.
To summarize, severe endometriosis causes infertility by distorting the anatomy of pelvic structures and interfering with ovulation by causing inflammation as an immunity response—the same kind of response your body sets into motion when you have any kind of disease it wants to fight off.
Scar tissue from endometriosis involving the fallopian tubes can lead to kinking or blockage of the tubes, making it difficult for eggs to travel down them or sperm to travel up. If the ovaries are surrounded by scar tissue, it is difficult for the eggs released during ovulation to be picked up by the tubes.
In patients with minimal or mild endometriosis, the implants release immune substances that interfere with hormones in the brain’s hypothalamus, the pituitary gland, and the ovaries. This can lead to local inflammation. Inflammation can harm ovarian response, quality of ovulation, egg quality, and egg-sperm interaction as well as implantation of an embryo in the uterus.
Ovarian cysts (endometrioma) are also associated with inflammation and have a negative impact on ovarian response and egg quality.
If you are having difficulty achieving pregnancy and you know (or suspect) that you have endometriosis, there is hope. With the right diagnosis, treatment and support, you can receive effective care for endo and greatly increase your chances of going on to conceive and carry a pregnancy to term.
All of the doctors at InVia Fertility Specialists are board-certified in reproductive endocrinology and infertility, with years of experience diagnosing and treating infertility caused by endometriosis.
If you are in the Chicago area, we have four convenient locations where you can meet with me and my colleagues Dr. Puscheck and Dr. Klipstein. Make an appointment online today by clicking the banner below.

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
