We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
Let me describe a common clinical situation to you. It goes like this:
My OB/GYN found a cyst in my ovary and she thinks it may be an endometrioma. Given that I have been trying to get pregnant for the past two years, she has referred me to an infertility specialist. What is an endometrioma? Can it be the cause of my infertility? Do I need surgery? What is the best option for me to get pregnant?
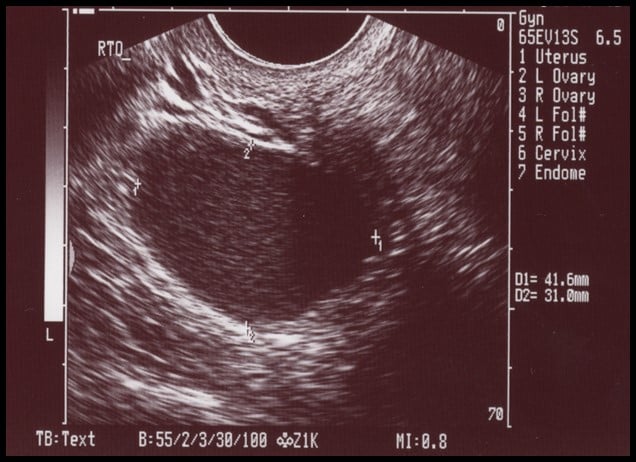
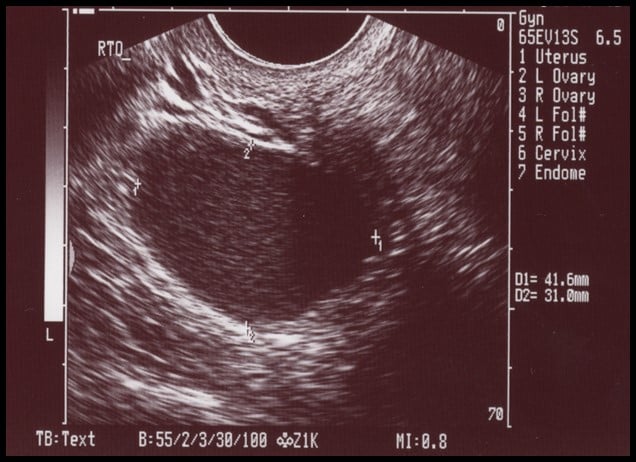
If you’re a fertility patient, you may be familiar with this scenario, and with the type of picture shown above. It’s an ultrasound image of a typical endometrioma, which is a cyst caused by endometrial tissue in the ovary. On the image, it appears to have a homogeneous “ground glass” appearance, meaning there are consistent low-level echos with smooth borders throughout the cyst—those light grey bumps or streaks within the central dark region.
Typically, an image that looks like this on ultrasound is 90% likely to be an endometrioma. However, there are some common “imposters”—other structures that can look like an endometrioma on ultrasound but turn out to be something else on further investigation. The most common imposter is a hemorrhagic corpus luteum cyst. So, what are both of these things and how can we tell the difference?
First, let me set your mind at ease: endometriomas and hemorrhagic corpus luteum cysts are both benign—that is, they’re not cancerous. This means we can take our time to evaluate these cysts noninvasively and conservatively by conducting repeat ultrasound investigations and by thinking about physiology.
Whenever you ovulate, a mature egg is released from a follicle in your ovary. The empty follicle left behind becomes a corpus luteum—Latin for “yellow body”, because this structure often takes on a yellowish color. If there is some bleeding into the corpus luteum, then it becomes a “hemorrhagic” corpus luteum. “Hemorrhagic” in this instance just means that there is some blood within the corpus luteum, not that it is freely or uncontrollably bleeding. A hemorrhagic corpus luteum cyst is therefore what we call a “functional” cyst—one that occurs as the result of a normal, natural process.
Hemorrhagic corpus luteum cysts are common. They may be associated with some pain, because the bleeding stretches the wall of the old follicle and then clots. If you have an ultrasound at this point, it may look just like an endometrioma to your ultrasound tech and your doctor. The difference is that the blood in a hemorrhagic corpus luteum will be absorbed and go away over time.
So, we will often wait one month and repeat the ultrasound near the time of your next period. If the cyst has disappeared, it was a hemorrhagic corpus luteum and has resolved naturally.
There are other mimics of endometriomas, too, but the hemorrhagic corpus luteum is a very common culprit!
An endometrioma is a form of endometriosis. Endometriosis is when the lining of the uterus (known as the endometrium) is found outside of the uterus. An endometrioma occurs when endometriosis invades the ovary and bleeds into the cyst. This blood is broken down and looks brown, which is why you will often hear endometriomas referred to as “chocolate cysts”.
The lining of this cyst consists of the glands and stroma of the endometrium and it does not go away over time. It may stay the same or get bigger.
The answer to this question depends on several factors. The first is how you are feeling. If you are in pain, then it should be removed, preferably preserving as much of the ovary as possible for your fertility.
If left alone, large cysts can rupture, cause torsion, or leak the “chocolate” fluid into the pelvis. The “chocolate” fluid contains broken-down products of blood and cytokines, which are inflammatory. This inflammatory fluid irritates the abdominal cavity walls and causes more pain. Your body may respond to this irritation by walling the endometrioma and your ovary off with scar tissue (adhesions).
If there is no pain, or if the pain is tolerable, we may choose to monitor the endometrioma as long as it is not too big. If the endometrioma is large or causing pain, surgery is probably on the cards.
Our greatest concern with endometrioma surgery is the potential loss of ovarian reserve—that is, damage to the ovary that can cause loss of eggs. Whenever endometrioma surgery is performed, there is a risk of some ovarian cortex being removed with the cyst. There may also be some damage to the remaining ovary if there is bleeding after we remove the cyst and we have to perform cauterization (burn the surface of the ovary to seal the wound and stop the bleeding).
Finally, there are some situations which can arise during surgery to remove an endometrioma which may lead to the removal of the entire ovary—though we try to avoid this if at all possible. If you are unfortunate enough to have a very large endometrioma, it’s more likely you will need to have the entire ovary removed. But even smaller endometriomas may have a lot of scar tissue around them, which can make this kind of surgery difficult. If there is significant bleeding due to removal of scar tissue, this can also mean a surgeon will need to remove the ovary.
Removing the ovary will also mean losing any eggs it contained, which will impact your fertility.
If we leave the endometrioma in place as we proceed with fertility treatment, it can continue to cause issues. This can include rupture of the cyst during ovarian stimulation or accidental drainage of the cyst during IVF retrieval and continued leakage. In these situations, there can be “chemical peritonitis”—inflammation which can cause pain and other issues.
There is also potential for ovarian torsion, meaning a twisting of the ovary which cuts off the blood supply. Torsion does not happen often since many endometriomas are associated with adhesions (scar tissue) which “stick” the ovary in place and make it less likely to twist. But if it does happen, ovarian torsion can quickly turn into an emergency situation requiring immediate attention and surgery.
Given these risks, is there a role for medication in treating an endometrioma? Typically, medical treatment used to suppress endometriosis involves reducing your estrogen level. First-line medical treatments for endometriosis (not endometriomas) consist of birth control pills (or other combined hormonal contraceptives).
Other medications work by shutting down the signaling pathway for the ovarian follicles to grow and make estrogen. These medications are known as GnRH agonists or, more recently, an oral GnRH antagonist (Elagolix). This newer medication is often given to suppress endometriosis and the pain associated with endometriosis if birth control pills do not work or if you cannot take them. It is easier and safer than the GnRH agonist (i.e. Lupron acetate), which usually comes in the form of monthly injections.
However, none of these medical treatments will resolve an endometrioma—they will just reduce pain and discomfort and prevent further spread of the endometriosis. So these medications tend to delay fertility treatments and do not reduce the time to pregnancy.
Endometriomas may have a classic appearance on ultrasound and this noninvasive approach to diagnosis may be 90% accurate. If an ultrasound shows a suspected endometrioma and you want to achieve a pregnancy, you should follow up with an infertility specialist for further evaluation and to discuss your treatment options.
Do not be surprised if the treatment is to proceed with infertility treatments while monitoring the endometrioma. This approach is very common and helpful in achieving pregnancy in many instances. Ironically, one of the best ways to reduce endometriosis overall is by taking a pregnancy to term!
Dealing with endometriosis, endometriomas and infertility can be a true balancing act. Please don’t hesitate to get in touch with me and my colleagues here at InVia Fertility Specialists if you want help with this tricky clinical situation. We are all experienced with treating endometriosis and the fertility issues it can cause. Click below to make an appointment at one of our four Chicago-area clinics!

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
