We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
We are experiencing a very high volume of calls and messages and ask for your patience. We will answer your portal messages within 48 hours.
 A vaginal egg collection is a very routine part of the IVF process. The procedure is over in about 20 minutes, and experienced doctors will usually get one egg from each mature follicle.
A vaginal egg collection is a very routine part of the IVF process. The procedure is over in about 20 minutes, and experienced doctors will usually get one egg from each mature follicle.
However, one complication that can mar a vaginal egg collection is empty follicle syndrome.
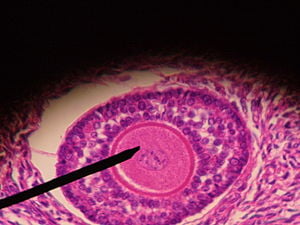
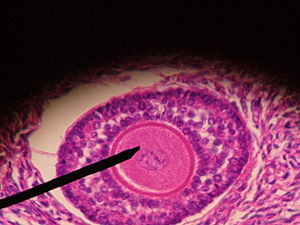
Egg collection consists of a number of routine steps: the doctor aspirates the follicles to collapse them, punctures the follicles, and the follicular fluid – presumably containing eggs – flows into test tubes. The follicular fluid is given to the embryologist to scan under a microscope, where the eggs are visible.
Empty follicle syndrome is detected when no eggs are visible under the microscope. This is unexpected and uncommon; and many doctors are completely stumped as to what to do when this happens. This is actually a medical emergency, but is often managed badly.
Sometimes the doctor will just continue with the procedure blindly, and suck out the follicular fluid from all the follicles. After they've completing the procedure and left the OR, the embryologist then reports to the doctor that no eggs were found. The doctor then must tell the patient – sorry, we did not get any eggs at all. It's typical for the patient to be stunned and / or in disbelief. The doctor may offer the use of donor eggs at this time, and the patient may feel bulldozed into agreeing, in order to salvage a bad situation.
How should a doctor manage the crisis of empty follicle syndrome?
It's important to realize that 99 percent of the time , empty follicle syndrome occurs because the patient has not taken the hCG injection properly. This could occur for multiple reasons. The patient may have forgotten to dissolve the powder in the solvent while taking the trigger shot, and taken only the inert solvent; or she may have taken an HMG injection instead of the hCG; or may have mis-timed it; or may have spilled the drug, and was too scared to tell the doctor what happened.
Proper management of empty follicle syndrome is as follows: Firstly, we use a double lumen needle for the egg collection, and flush each and every follicle at least 4 times, with the expectation of finding one egg in each follicle. However, if the embryologist does not get any eggs after we have flushed three mature follicles, we stop the procedure.
We do a detailed analysis, in order to ensure that the patient has taken the trigger injection at the right time. In order to make diagnosis of empty follicle syndrome we use a rapid home pregnancy test kit in order to check the urine (obtained by catherisation) for the presence of hCG. (Instead of urine, it's also possible to do the test on the aspirated follicular fluid.) If the patient has taken her hCG properly , we would expect to find a positive pregnancy test. This rules out the diagnosis of empty follicle syndrome, and we can then continue with the egg collection.
However, if the pregnancy test is negative, the diagnosis of empty follicle syndrome is confirmed. At this point we stop the procedure, leaving the rest of the follicles intact, and wheel the patient out of the OR. We give the patient an additional HMG injection to support follicular growth. and do a blood test to measure estrogen and hCG levels. (Remember that we will get the results of the blood tests only after a few hours.)
We then give the patient another hCG injection, and reschedule the egg collection 36 hours after this second hCG shot. If we are worried about the quality of the hCG injection, we may use recombinant hCG (such as Ovitrelle) to trigger ovulation, and we may also increase the dose of hCG to 20000 IU (instead of the standard 10000 IU we use routinely).
The next day, we review the blood test results. We would expect the estradiol levels to be high and the hCG level to be less than 100 mIU/ml, thus confirming the diagnosis of EFS. An ultrasound scan at this time confirms that the follicles are still intact.
At the time of the second egg retrieval, which is planned 36 hours after the second hCG shot, we expect to see intact follicles and expect to retrieve eggs from each of these follicles. In order to document the diagnosis, we repeat the blood hCG level again and expect this to be more than 100 mIU/ml.
Using this protocol, it is possible to salvage the situation, and give the patient a very good chance at getting pregnant !

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
