
-4.jpg?width=300&name=My%20Post%20(3)-4.jpg) What is adenomyosis?
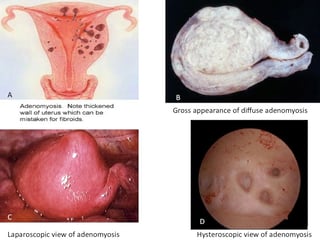
What is adenomyosis?Adenomyosis is defined as the presence of endometrial tissue, which normally lines the uterus, which has grown into the muscular wall of the uterus. It can be diffuse or localized (focal) and the lesions can be solid or cystic.
Adenomyosis differs from endometriosis — a condition in which the uterine lining becomes implanted outside the uterus — although women with adenomyosis often also have endometriosis.
In endometriosis, the “functional” part of the uterine lining is implanted – these implants respond to the (monthly) cyclical changes in your hormone levels. In adenomyosis the “basal” layer of the uterine lining grows within the uterine musculature. The basal lining is NOT responsive to cyclical changes in your hormone levels. The cause of adenomyosis remains unknown, but the disease typically disappears after menopause.
-4.jpg?width=300&name=My%20Post%20(3)-4.jpg) What is adenomyosis?
What is adenomyosis?
Adenomyosis is defined as the presence of endometrial tissue, which normally lines the uterus, which has grown into the muscular wall of the uterus. It can be diffuse or localized (focal) and the lesions can be solid or cystic.
Adenomyosis differs from endometriosis — a condition in which the uterine lining becomes implanted outside the uterus — although women with adenomyosis often also have endometriosis.
In endometriosis, the “functional” part of the uterine lining is implanted – these implants respond to the (monthly) cyclical changes in your hormone levels. In adenomyosis the “basal” layer of the uterine lining grows within the uterine musculature. The basal lining is NOT responsive to cyclical changes in your hormone levels. The cause of adenomyosis remains unknown, but the disease typically disappears after menopause.
Adenomyosis can sometimes be without any signs or symptoms. In other cases, adenomyosis may cause:
Your uterus may double or triple in size. Although you might not know if your uterus is enlarged, you may notice that your lower abdomen seems bigger or feels tender.
Any and all of these symptoms can contribute towards lowering your quality of life;
The cause of adenomyosis isn’t known. Expert theories about a possible cause include:
Regardless of how adenomyosis develops, its growth depends on the circulating estrogen in a woman’s body. When estrogen production decreases at menopause, adenomyosis eventually goes away.
Adenomyosis is increased after uterine surgery (e.g. removal of fibroids), cesarean delivery, infections after delivery (post partum endometritis), pregnancy, other uterine manipulations (D&C, endometrial ablation).
Your doctor may suspect adenomyosis based on:
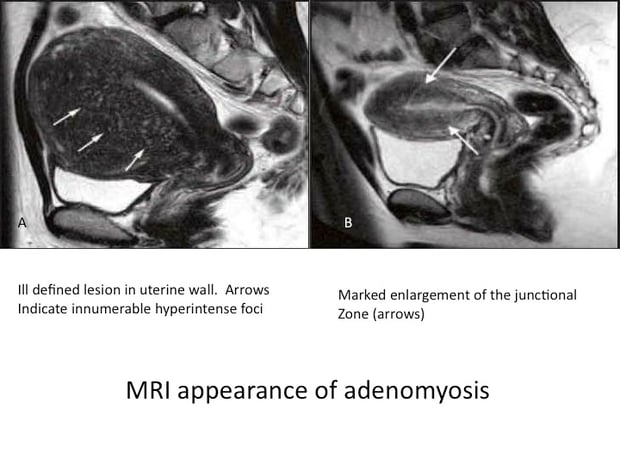
In some instances, your doctor may biopsy a small piece of your uterine lining to rule out cancer. However, such a biopsy won’t help your doctor confirm a diagnosis of adenomyosis. The only way to be certain of adenomyosis is to examine uterine tissue using a microscope after removal of the uterus (hysterectomy).
Many women have other uterine diseases that cause signs and symptoms similar to adenomyosis, making adenomyosis more difficult to diagnose. Such conditions include fibroid tumors (leiomyomas), uterine cells growing outside the uterus (endometriosis) and growths in the uterine lining (endometrial polyps). Your doctor may diagnose adenomyosis only after he or she determines there are no other causes for your signs and symptoms.
There is no definite established causal relationship between adenomyosis and infertility. A recent publication in the journal Human Reproduction (Vercellini et al. Vol.29, No.5 pp. 964–977, 2014) showed a 28% reduction in IVF pregnancy rates in patients with adenomyosis. There was also an increase in the miscarriage rate and a decrease in the live birth rate.
The treatment is usually symptomatic. This includes the use of anti-inflammatory medications (Motrin, Advil. Ibuprofen) for symptomatic relief. Birth control pills may be prescribed to control bleeding. Use of medications to suppress the adenomyosis (GnRH agonists e.g. leuprolide acetate (Lupron) or nafarelin (Synarel)) has met with limited success.
A hysterectomy is a reasonable option for women who have completed child bearing. However, patients desiring fertility can be offered uterus-sparing surgeries. In this the adenomyosis is surgically removed and the uterus is then reconstructed. Unlike fibroids (that have a capsule and therefore can be easily shelled out), adenomyosis resection can be surgically challenging.

Entire Website © 2003 - 2020
Karande and Associates d/b/a InVia
Fertility Specialists
