Good eggs and a healthy embryo aren't enough to assure pregnancy during IVF. A receptive uterine lining (endometrium) is also critical for successful implantation after embryo transfer. A commonly used parameter for assessing the endometrium is to measure its thickness (endometrial thickness, EMT).
 During the stimulation phase of IVF, EMT usually increases in response to estrogen released by the ovaries. EMT is now routinely measured using transvaginal ultrasound during in vitro fertilization (IVF).
During the stimulation phase of IVF, EMT usually increases in response to estrogen released by the ovaries. EMT is now routinely measured using transvaginal ultrasound during in vitro fertilization (IVF).
Some studies have suggested that a thin lining is associated with low IVF pregnancy rates, whereas others were not able to confirm this. Despite this, it is generally accepted that a "thick" lining will be most receptive for the embryo(s) after transfer.
Here are ten facts you will probably want to know if you have questions about EMT:
- The most commonly used cut-off for defining a thin endometrium is less than or equal to 7 mm.
- In a recent review of the literature (Kasius et al. Human Reproduction Update, Vol 20, No. 4 pp 530 – 541, 2014) in which 1170 studies were analyzed, a thin endometrium was reported in only 2.4% of cases where pregnancy occurred.
- The probability of clinical pregnancy for an EMT less than or equal to 7 mm was significantly lower compared with cases with EMT greater than 7 mm (23.3% versus 48.1%, OR 0.42 (95% CI 0.27 – 0.67).
- EMT has no predictive value for the occurrence of pregnancy. Meaning, it is not possible to predict who will and who will not get pregnant based on endometrial thickness alone.
- In patients with thin endometrium, it is the basal layer of the endometrium that is predominant as the functional layer has not developed. The basal layer has an increased blood supply and oxygen concentration. High oxygen levels may be detrimental for embryo implantation.
- EMT measurements can vary by as much as 1.5 mm based on the technique used by the person performing the ultrasound. Meaning, if two different individuals measure the same lining, the EMT measurement can vary. Also, differences in equipment (including resolution of ultrasound machines) could cause differences in EMT measurements.
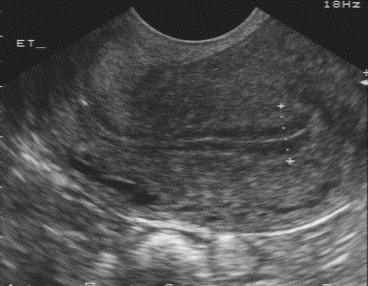
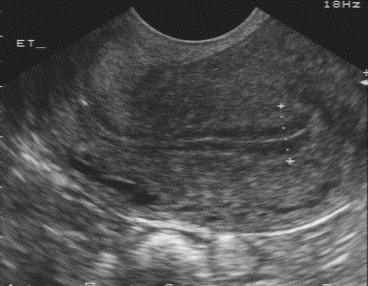
The technique of measuring EMT is critical. When using a vaginal-probe ultrasound, it is important that the bladder be empty and the patient should be positioned so that manipulation of the transducer is possible. The endometrium should be measured in the long-axis or saggital plane. The measurement is of the thickest echogenic area from one basal endometrial interface across the endometrial canal to the other basal endometrium. Care should be taken not to include the hypoechoic myometrium in the measurement (see picture above).
- There are multiple causes of a thin endometrium. Intrauterine adhesions can cause the lining to be thin. These need to be ruled out with a hysterosonogram, hysterosalpingogram or hysteroscopy prior to starting an IVF cycle. In patients with a normal cavity, it is believed that the functional layer of the endometrium does not develop leading to a thin lining.
- The impact of endometrial patterns on IVF pregnancy rates has been investigated, once again with conflicting results.
- Treatment strategies include freezing all the embryos and doing a cryo-preserved embryo transfer cycle. There is no universally agreed EMT below which freezing all embryos is mandatory. At InVia, we will consider this option when the EMT is less than 4 mm.
- One group of researchers investigated Viagra vaginal suppositories to support endometrial thickness. The dose is one 20 mg Viagra suppository to be inserted high in the vagina starting after menses and continuing till the hCG trigger. 75% of women were reported to show improvement in the lining with 2 - 3 days. Other groups need to confirm this finding. The instillation of growth factors (Neupogen or G-CSF) is also being investigated.
Make an appointment at one of InVia’s four Chicago area fertility clinics to speak with a board-certified, compassionate physician who wants to help you on your path to pregnancy.

 During the stimulation phase of IVF, EMT usually increases in response to estrogen released by the ovaries. EMT is now routinely measured using transvaginal ultrasound during in vitro fertilization (IVF).
During the stimulation phase of IVF, EMT usually increases in response to estrogen released by the ovaries. EMT is now routinely measured using transvaginal ultrasound during in vitro fertilization (IVF). 
